Health
Urgent Call for Reform in UK End-of-Life Care Funding
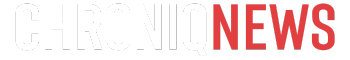
The state of end-of-life care in the United Kingdom faces a looming crisis, as funding shortages threaten the quality of services available to those in need. Currently, the National Health Service (NHS) funds only about 30% of hospice care, leaving a significant gap that is primarily filled by charitable donations. According to a recent report from the National Audit Office, approximately two-thirds of adult hospices in England reported deficits for the fiscal year 2023-24. This underfunding is leading to staff cuts, reduced bed availability, and diminished community services, creating a troubling disparity in care quality based on geographic location.
The reality is stark. For instance, in a recent announcement, the Arthur Rank Hospice in Cambridgeshire revealed that Cambridge University Hospitals would withdraw £829,000 in annual funding, resulting in the closure of nine out of twenty-one hospice beds. This reduction means that over 200 individuals per year will be deprived of the option to receive care in a more comforting environment, forcing them instead into busy hospital settings. Sharon Allen, CEO of Arthur Rank, expressed her concerns, stating that the decision reflects a troubling perspective on the value of hospice care.
The implications of inadequate funding extend beyond financial metrics. For healthcare professionals like Dr. Rachel Clarke, a specialist in palliative medicine, the impact is deeply personal. Daily encounters with patients reveal the harsh realities of insufficient resources. “I’m so sorry, there are still no beds at the hospice,” has become a familiar refrain that echoes the frustrations of families during critical moments.
The crisis in palliative care highlights a significant disparity between the treatment of terminally ill patients and that of infants requiring neonatal care. While the NHS has been recognized as a core service for pediatric care, the same cannot be said for end-of-life services. This inconsistency raises questions about societal values and the collective response to the needs of the dying.
As demand for palliative care is projected to increase by more than 25% by 2048, urgent action is necessary. The debate surrounding assisted dying, with the Kim Leadbeater bill currently progressing through the House of Lords, underscores the importance of ensuring high-quality palliative care remains accessible. Currently, around 150,000 individuals annually are unable to access the palliative care they require, leading to a troubling scenario where some may feel compelled to consider assisted dying due to lack of support.
The government’s response to the ongoing crisis has been criticized for its lack of urgency. A recent statement acknowledged the need for improvement but offered little in terms of concrete action. The NHS 10-Year Plan for England mentions “palliative” only once, reflecting a systemic oversight in addressing the needs of those at the end of life.
The conversation surrounding end-of-life care must evolve. As a society, there is a collective obligation to confront the realities of mortality and advocate for comprehensive palliative care. By fostering an environment that prioritizes dignity and compassion in dying, the UK can move toward a more humane approach to end-of-life experiences.
In summary, the current state of palliative care funding in the UK presents a critical challenge that cannot be ignored. With a growing population of individuals facing terminal illnesses, it is time for policymakers and the public alike to demand better resources and support for end-of-life care. Only through concerted effort can we ensure that every individual receives the dignity and care they deserve in their final days.
-

 Top Stories2 weeks ago
Top Stories2 weeks agoMarc Buoniconti’s Legacy: 40 Years Later, Lives Transformed
-
 Health3 weeks ago
Health3 weeks agoInnovative Surgery Restores Confidence for Breast Cancer Patients
-

 Sports4 weeks ago
Sports4 weeks agoSteve Kerr Supports Jonathan Kuminga After Ejection in Preseason Game
-

 Science4 weeks ago
Science4 weeks agoChicago’s Viral ‘Rat Hole’ Likely Created by Squirrel, Study Reveals
-

 Politics4 weeks ago
Politics4 weeks agoDallin H. Oaks Assumes Leadership of Latter-day Saints Church
-

 Lifestyle4 weeks ago
Lifestyle4 weeks agoKelsea Ballerini Launches ‘Burn the Baggage’ Candle with Ranger Station
-

 Entertainment4 weeks ago
Entertainment4 weeks agoZoe Saldana Advocates for James Cameron’s Avatar Documentary
-

 Top Stories2 weeks ago
Top Stories2 weeks agoBOYNEXTDOOR’s Jaehyun Faces Backlash Amid BTS-TWICE Controversy
-

 Business4 weeks ago
Business4 weeks agoTyler Technologies Set to Reveal Q3 2025 Earnings on October 22
-

 Business3 weeks ago
Business3 weeks agoZacks Research Downgrades Equinox Gold to Strong Sell Rating
-

 Health4 weeks ago
Health4 weeks agoCommunity Unites for Seventh Annual Mental Health Awareness Walk
-
 Health3 weeks ago
Health3 weeks ago13-Year-Old Hospitalized After Swallowing 100 Magnets